Dr. Amy Case and colleagues create dosing table to guide use of opioid shown to have low dependence potential
BUFFALO, N.Y. — Opioid painkillers are very effective when used to manage cancer-related pain, but they’re also highly addictive. Because abuse and misuse of this class of drugs is common, and because opioid overdose is the leading cause of accidental death in New York State, doctors who treat patients with cancer face unique challenges when prescribing pain relievers.
To help overcome this challenge, a Roswell Park Comprehensive Cancer Center-led team recently compiled a literature review and clinical recommendations to guide clinicians on use of buprenorphine, a schedule III opioid, for effective relief from pain caused by cancer or cancer treatment. The team published the resource as a review article in Current Treatment Options in Oncology, and also shared their recommendations at the annual meeting of the American Academy of Hospice and Palliative Medicine.
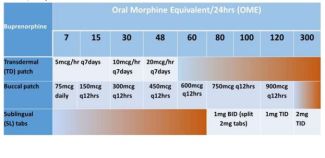
Because there is limited guidance on the appropriate use of buprenorphine for chronic pain management, the review article, “Treating Chronic Pain with Buprenorphine: The Practical Guide,” introduced a novel conversion table to help clinicians switch their patients from a traditional opioid to buprenorphine.
“In the age of the opioid epidemic, there is demand for an analgesic that has less abuse potential and adverse side effects compared with other opioids,” says Amy Case, MD, FAAHPM, the Lee Foundation Endowed Chair of Palliative and Supportive Care and Palliative Care Program Chief at Roswell Park, who speaks nationally on the use of buprenorphine, an opioid with unique properties that make it useful in a variety of different clinical scenarios. “Buprenorphine is an opioid with less potential for abuse and a lower risk of adverse effects such as sedation or cognitive impairment, but few palliative care providers are well versed in this drug.”
Buprenorphine was introduced in the United States in 1981 as an injectable schedule V pain reliever under the Controlled Substances Act. In 2002, a sublingual (applied under the tongue) formulation was approved for opioid dependence and reclassified as a schedule III drug. In 2010, a transdermal buprenorphine patch was approved for pain management, and in 2019, the U.S. Department of Health and Human Services released a new set of pain guidelines that recommended the use of buprenorphine as a first-line opioid for chronic pain in cases where an opioid is needed.
Today, buprenorphine is available in more than 40 countries, but its use is fairly limited to a second- or third-line opioid for pain that can’t be effectively controlled using other agents. The drug is also sometimes used for maintenance or discontinuation therapy in patients who are addicted to opioids.
Despite its limited use, buprenorphine has several advantages over other painkillers, including a lower incidence of depression, and it appears to be less addictive than traditional opioids. The drug offers effective pain relief, with 85% of patients reporting pain control to be good or very good. An additional advantage is that other opioids can be used in addition to buprenorphine for cases of breakthrough pain.
“The drug’s unique pharmacological properties make it an attractive first-line opioid for chronic pain, especially in older patients, as it results in less sedation or cognitive impairment when compared with other opioids, reducing the risk of confusion or falls,” says Dr. Case.
Buprenorphine also has better tolerability, fewer side effects, and a better safety profile than other opioids. Compared with other opioids, buprenorphine is safer to use in patients with mild to moderate kidney disease, renal insufficiency, and mild to moderate liver disease.
“The popularity of using buprenorphine for analgesia continues to grow over time and with practice,” says Dr. Case. “This drug should be considered as an excellent and safe option for the management of acute and chronic pain.”
###
Roswell Park Comprehensive Cancer Center is a community united by the drive to eliminate cancer’s grip on humanity by unlocking its secrets through personalized approaches and unleashing the healing power of hope. Founded by Dr. Roswell Park in 1898, it is the only National Cancer Institute-designated comprehensive cancer center in Upstate New York. Learn more at www.roswellpark.org, or contact us at 1-800-ROSWELL (1-800-767-9355) or ASKRoswell@RoswellPark.org.